Chronic Osteomyelitis: Diagnosis and Treatment
Машинный перевод
Оригинальная статья написана на языке RU (ссылка для ознакомления) .
Osteomyelitis of the jaw is an infectious purulent-necrotic process that develops in the bone and bone marrow of the jaw, as well as in the surrounding soft tissues against the background of prior sensitization of the body. In this article, we will discuss chronic osteomyelitis of the jaw, the features of diagnosis and treatment.
More about this topic in the webinar Odontogenic Osteomyelitis of the Jaws.
Chronic Osteomyelitis of the Jaw
Chronic osteomyelitis of the jaw develops from an untreated acute form of the disease. This type of osteomyelitis is called secondary-chronic. If the inflammatory process was initially sluggish and not as pronounced clinically as acute, then it is primary-chronic osteomyelitis.
Chronic osteomyelitis, like acute, can be of infectious and non-infectious origin. The former is further divided into odontogenic and non-odontogenic.
According to the predominance of processes of formation or destruction of bone substance, three clinical-radiological forms of chronic odontogenic osteomyelitis of the jaws are distinguished: productive (without sequestrum formation), destructive (with sequestrum formation), and destructive-productive. The productive form is less common than the others, mainly occurring at a young age.
Chronic Odontogenic Osteomyelitis of the Jaw
Chronic odontogenic osteomyelitis of the jaw is more often secondary-chronic and is considered a complication of acute odontogenic osteomyelitis. The transition from the acute stage of the disease to the chronic stage typically occurs in the 4th to 5th week of the disease. By this time, the manifestations of acute inflammation subside: the swelling of the soft tissues surrounding the jaw decreases, the amount of pus discharged from the wound decreases, the pus itself becomes thicker, and granulation tissue forms in the wound.
The overall condition of the patient also normalizes: body temperature returns to normal, the patient does not complain of pain in the affected area, sleep and appetite are restored, and blood tests approach normal values.
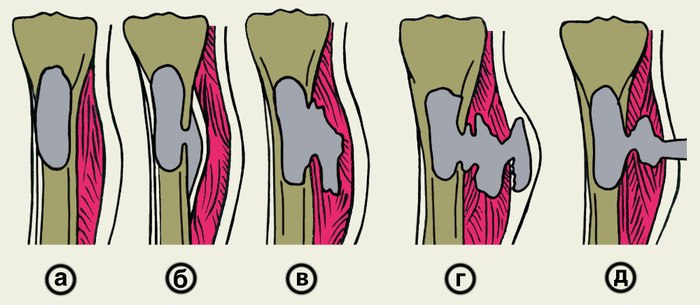
Figure 1. Formation of a fistulous tract.
The first clinical sign that the acute stage has not been cured is the appearance of fistulas with pus in the area of the wound. Sometimes fistulas may open on the skin of the jaw and face area.
Next, sequestra formation is observed, which, depending on their size, either exit through the fistulous tracts (small ones) or need to be removed by a maxillofacial surgeon (large ones).
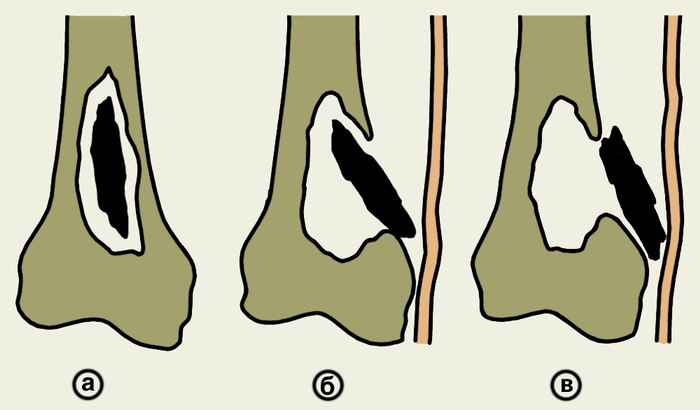
Figure 2. Formation and rejection of sequestrum.
When the outflow of pus is disrupted and small sequestra are not removed through the fistulous tracts, the chronic process exacerbates, and the clinical picture becomes the same as in acute osteomyelitis.
The picture described above is characteristic of the destructive or destructively-productive forms of osteomyelitis. The productive form is characterized by the absence of sequestra and an increase in bone tissue in the area of inflammation, occurring only in osteomyelitis of the mandible.
Diagnosis of Chronic Odontogenic Osteomyelitis
The diagnosis of chronic odontogenic osteomyelitis involves collecting the patient's medical history, examining the patient, and performing radiography.
From the medical history, we learn that the patient either suffered from acute osteomyelitis and did not seek help, or assistance was provided, but the acute form of the process transitioned to chronic. In both cases, further examination of the patient is conducted.
The clinical picture is very diverse, making it difficult to accurately characterize all the signs of the disease.

Externally, the face may appear asymmetrical due to soft tissue swelling or bone tissue deformation. In the productive form, asymmetry may be caused by an increase in the volume of bone tissue.
The mouth opening is either normal or not fully achieved, which is caused by inflammatory contracture of the masticatory muscles.
Lymph nodes are normal or may be slightly enlarged and painful upon palpation.
During the examination of the oral cavity, an inflammatory infiltrate is identified, hyperemic mucosa, the causative tooth or the socket of the extracted tooth. Fistulas are found on the mucous membrane of the oral cavity or on the skin, through which formed sequestra are probed. Teeth are less mobile in the chronic form of the disease compared to acute osteomyelitis.
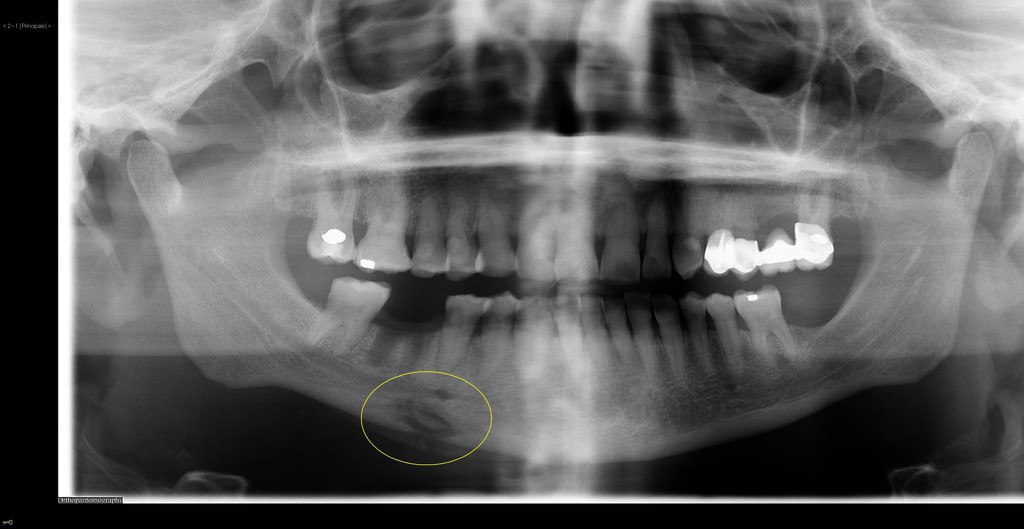
Next, radiodiagnostics are performed, preferably orthopantomography or X-ray imaging in two projections (frontal and lateral). In the acute form of odontogenic osteomyelitis, only the focus of infection is observed – rarefaction of bone tissue in the area of the apex of the causative tooth. If the disease has progressed to a chronic form, sequestra are visible on the X-ray. However, the first manifestations of the disease appear on the X-ray only by the end of the 2nd, and sometimes the 3rd week. The above describes the situation in the destructive form of osteomyelitis.
If we talk about the productive form, sequestration of the bone is not noted. However, the amount of mineralized tissue increases due to the reaction of the periosteum. The patient's face becomes asymmetrical, and the bone increases in volume.

Chronic Odontogenic Osteomyelitis of the Mandible
Chronic odontogenic osteomyelitis of the mandible more often affects only the alveolar part of the bone, less frequently the body or ramus of the mandible. Due to the peculiarities of its structure, the disease progresses severely with the formation of small and large sequestra. Often, destruction of the bone tissue leads to a pathological fracture (the bone breaks with a weak "impact" on the jaw).
Chronic Odontogenic Osteomyelitis of the Maxilla
Chronic odontogenic osteomyelitis of the maxilla develops faster and is milder than that of the mandible. Sequestra form within 3-4 weeks, while in the mandible it takes 6-8 weeks. In the diffuse form of the disease, destruction of the anterior wall of the maxillary sinus or even the lower edge of the orbit may occur.
Treatment of Chronic Odontogenic Osteomyelitis of the Jaw
The treatment of chronic odontogenic osteomyelitis of the jaw is comprehensive, including surgical intervention and medication.
I. During an exacerbation of chronic osteomyelitis, the symptoms of acute inflammation are first alleviated. If the causative tooth has not been previously removed, it should be extracted this time. Adjacent mobile teeth are trephined and splinted if they are not removed for indications (after assessing their viability and conducting X-ray examination). Oral cavity sanitation is mandatory, and all chronic sources of infection are removed to prevent complications during subsequent procedures.
To facilitate the drainage of pus, fistulas or wounds are expanded, and primary surgical treatment of purulent foci is performed.
An important part of the surgical stage of treatment is sequestrectomy. After evaluating the X-ray, the removal of formed sequestra is carried out. The removal is performed through intraoral or extraoral incisions. Large sequestra in the body and ramus of the mandible, as well as in the area of the infraorbital rim and zygomatic bone, are removed extraorally. Sometimes large necrotized areas of bone are broken into several pieces for easier removal. Incisions are made along the natural folds of the face for better aesthetics.
After the removal of sequestra, attention is paid to granulations and the sequestral capsule. Pathological tissues are removed with a curette or even a drill until signs of healthy bone are observed: socket bleeding, white color of the bone, hard bone tissue.
The free space is filled with a biosynthetic osteotropic preparation: colapol, colapan, etc. The wound is tightly sutured, and drainage is left. The stitches are removed after 7-10 days.
II. Next, we will move on to drug treatment. As with other purulent diseases, etiological, pathogenetic, and symptomatic treatment is carried out.
To eliminate the cause of the disease, the surgeon removes the causative teeth. However, the infection remains in the blood, so the patient is prescribed antibacterial drugs: macrolides, cephalosporins. It is also advisable to prescribe antifungal agents to the patient.
Since the patient's immunity is reduced, the appointment of immune preparations such as thymalin, T-activin, levamisole, and staphylococcal anatoxin is recommended.
In cases of extensive bone tissue damage, a gentle diet is recommended for the patient to prevent pathological jaw fractures.
To reduce the symptoms of inflammation, detoxification and anti-inflammatory therapy are carried out. Individual exercises for therapeutic physical training and physiotherapy are selected for the patient to restore functions.
Chronic osteomyelitis of the jaw. Outcomes and complications
Outcomes:
- Favorable — with timely referral of the patient to the maxillofacial surgeon and adequate treatment, complete recovery of the patient is possible.
- Unfavorable – with insufficient treatment and late referral of the patient to the doctor, complications may occur.
In the event of an unfavorable outcome, the following may occur:
- exacerbation of the disease,
- deformation of the jaw,
- jaw fracture — occurs with minor physical impact that a healthy jaw would not have suffered from.
Complications of osteomyelitis:
- abscesses and phlegmons of the soft tissues of the face,
- thrombosis of the facial vessels and cavernous sinus,
- mediastinitis,
- fatal outcome.
Prevention of jaw osteomyelitis
The prevention of jaw osteomyelitis involves treating caries and its complications as sources of infection, timely visits to the dentist, periodic dental check-ups for preventive examinations, and strengthening the overall health of the patient.
For more relevant information, visit the section of our website Training in Oral and Maxillofacial Surgery.