Eminectomy of the temporomandibular joint
Машинный перевод
Оригинальная статья написана на языке PT (ссылка для ознакомления) .
Introduction
The temporomandibular joint (TMJ) is considered one of the most complex in the human body. The bony structures of the TMJ are the glenoid cavity of the temporal bone and the mandibular condyle. In children, the glenoid cavity and the articular eminence are flattened, with the action of functional loads being decisive in defining the morphology of the TMJ (Liddell & Perez, 2015; Martins et al., 2014; Mayrink et al., 2012; Undt, 2011).
During the movement of opening the mouth, the condyle has a rotational movement and subsequently an anterior translational movement, ideally to the point of greatest convexity of the articular eminence (Liddell & Perez, 2015; Martins et al., 2014; Mayrink et al., 2012; Undt, 2011).
Interposed between these bony surfaces is the articular disc, a biconcave, flexible structure made of fibrocartilaginous connective tissue, responsible for absorbing functional impacts and allowing the movement of the condyle to be harmonious during the opening and closing of the mouth (Pereira et al., 2021).
The pronounced anatomy of the articular eminence can represent a problem for the normal functioning of the TMJ. In this situation, the patient may present a limitation in the movement of mouth opening as the mandibular condyle does not traverse the inclination of the articular eminence.
In 1951, Hilmar Myrhaug introduced the surgical technique of eminectomy; this consists of reducing the height of the articular eminence so that the condyle can move freely without interference during the opening and closing of the mouth (Chakraborty, 2007; Liddell & Perez, 2015; Mayrink et al., 2012; Stassen & O’Halloran, 2011; Undt, 2011).
Case Report
A. S., a 20-year-old male patient, was observed during the first consultation for orofacial pain and temporomandibular dysfunction with nonspecific pain symptoms of moderate to severe intensity in the cervicofacial region without an apparent triggering factor. The patient described the presence of clicks, crepitations, and repeated episodes of locking during mouth opening. The entire existing clinical condition had an impact of 7/10 Visual Analogue Scale (VAS) on his quality of life.
Upon objective examination, we observed a maximum oral opening of 14 mm without deviations, presence of clicks, and bilateral muscle contracture with: grade 3 contracture in the masseter and temporal muscles and grade 2 in the sternocleidomastoid muscles and the anterior belly of the digastric muscle.
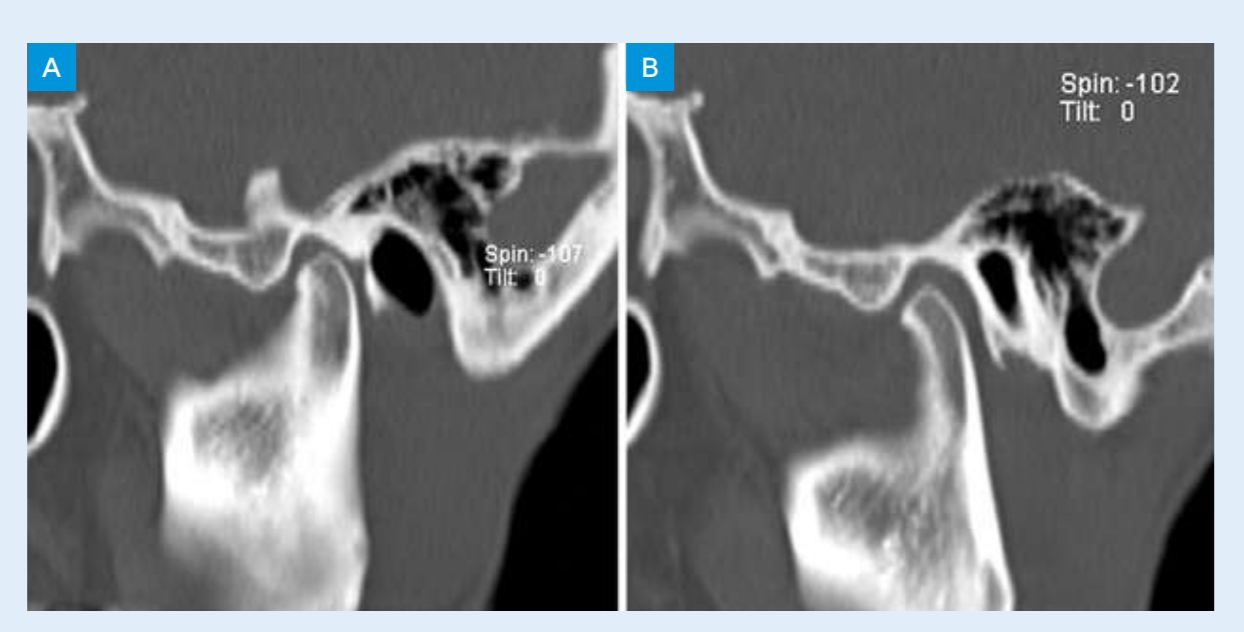
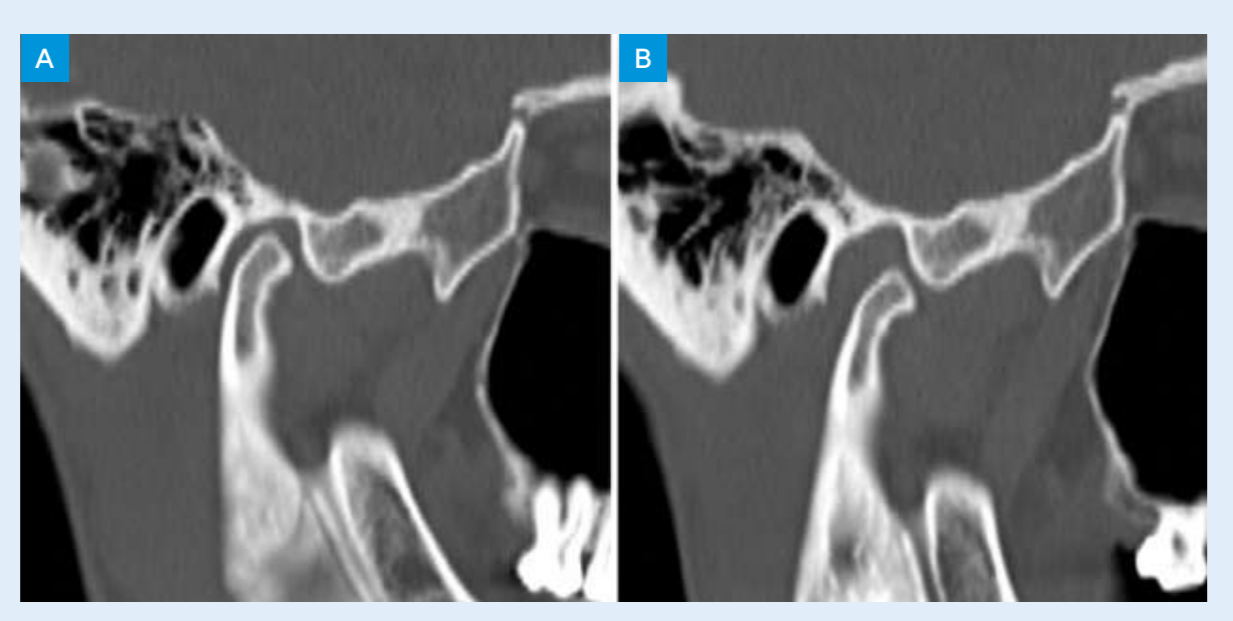
Complementary diagnostic exams were performed, with magnetic resonance imaging (MRI) showing good positioning of the discs with the mouth closed; however, with the mouth open, a posterior displacement of the articular discs was observed. The computed tomography (CT) revealed a very acute angle of the articular eminence that was associated with the blockage of condylar translation and the posterior displacement of the disc. In figures 1 and 2, the CT images with the mouth open and closed of the right and left TMJ can be seen.
The patient was proposed for bilateral eminectomy.
Description of the surgical technique of eminectomy
The most common approach in open TMJ surgery is the preauricular incision, described by Rowe in 1972. However, with the need for a more aesthetic approach, it has been replaced by an endaural approach and, more recently, a nomenclature has been proposed for a modification of the classic endaural approach: “Root of helix inter tragus notch incision (RHITNI).” This incision is made with a #15 blade and is drawn from the lower edge of the helix to the root of the ear, creating a V shape and continuing to the lower edge of the tragus, ending at the ear notch (Ângelo, 2020).
The dissection of the skin and subcutaneous tissues was performed with iris scissors, up to the superficial layer of the temporal fascia. After good exposure of the fascia, it was opened up to the zygomatic arch at a 45° angle to minimize the risk of injury to the temporal branch of the facial nerve (see figure 3). To reduce the articular eminence, the osteotomy was marked with a dermographic pen (see figure 4). The reduction of the articular eminence was performed atraumatically with the piezoelectric device (see figure 5).



The closure of the surgical wound was performed in layers, with 3/0 vicryl suture at the subcutaneous level and 5/0 monocryl suture for the skin. For protection, surgical glue was also applied over the entire suture and was removed twenty days after the surgery.
The entire surgery proceeded without complications, with an immediate postoperative maximum oral opening of 31 mm and adequate condylar translation recorded.
The patient was followed up with physiotherapy sessions and speech therapy sessions.
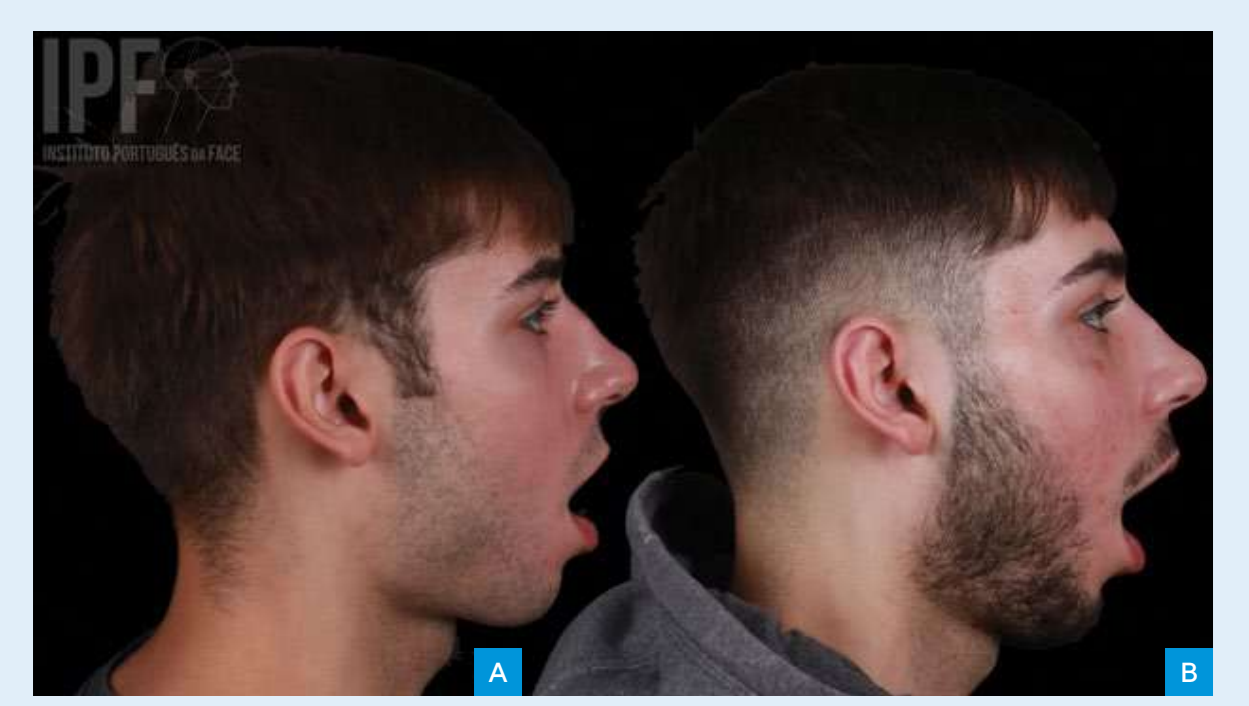
In figure 6(A) and 6(B) it is possible to observe the pre-operative profile photograph of the patient and six months after the surgery in maximum mouth opening.
Discussion
The eminectomy is a versatile technique in the treatment of different types of patients with TMJ pathology. Several authors describe eminectomy with an efficacy of 100% up to 5 years (Mayrink et al., 2012; Tocaciu et al., 2019).
The intervention is generally performed under general anesthesia, although some authors describe this procedure being done with local anesthesia and intravenous conscious sedation (Mayrink et al., 2012; Stassen & O’Halloran, 2011).
The reduction of the articular eminence can be performed using chisels, rotary drills, or reciprocating bone files, or, in a more recent approach, using piezoelectric devices. The main advantage of piezoelectric devices is the precision of the cut and the fact that it is atraumatic, preserving the integrity of vascular or nerve structures. Several authors have also reported a reduction in postoperative complications with piezoelectric devices compared to conventional surgery (Isler et al., 2018; Undt, 2011). The height of bone to be reduced is still not defined in the scientific community. Some authors recommend complete resection of the eminence, while others indicate only height reduction or partial contouring of the eminence (Undt, 2011). In our experience, a functional reduction of the eminence is performed, defined by a progressive reduction until we achieve an ideal translation.
In the scientific literature, some complications of eminectomy are described, such as injury to the facial and trigeminal nerves or damage to adjacent structures. Some authors observed persistence of mandibular dislocation, osteoarthritis, fracture of the condylar head, lateral deviation in the opening movement, and condylar hypermobility (Isler et al., 2018; Liddell & Perez, 2015; Martins et al., 2014).
Although condylar hypermobility is expected due to the absence of the articular eminence to contain the movement of the condyle, a study by Undt et al. did not show changes in joint movements in the pre or postoperative period; the authors mention the presence of a fibrous scar in the anterior sector of the capsule as a probable cause that prevents excessive movement of the condyle. A study by Stanssen et al. reports that none of the patients presented dysfunction resulting from postoperative hypermobility. Furthermore, none of the patients experienced problems with chewing, swallowing, or speaking (Mayrink et al., 2012; Stassen & O’Halloran, 2011; Undt, 2011).
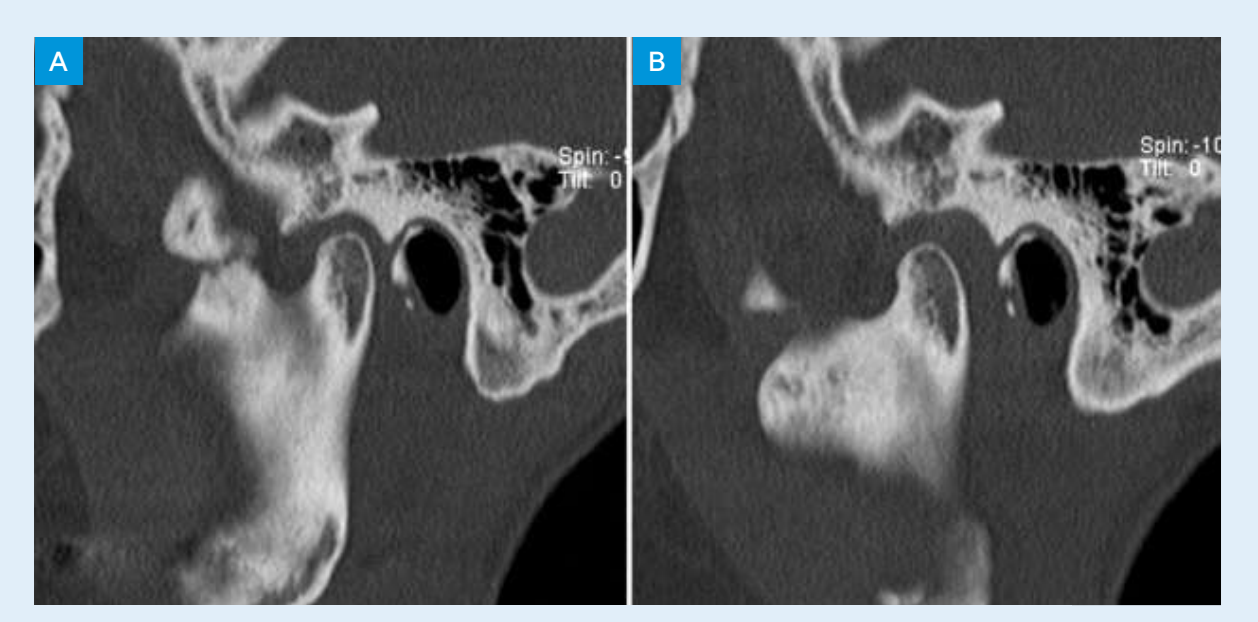
In our experience, a controlled and expected hypermobility was observed, which was decisive in improving mouth opening and in the passive repositioning of the disc. After a year, the patient underwent a new CT scan where the remodeling of the bilateral articular eminence could be verified, as seen in figures 7 and 8.

Conclusions
The eminectomy appears to be a safe and effective technique, associated with a rapid functional recovery with minimal aesthetic impact, due to the evolution of surgical techniques.
David Ângelo, David Sanz, Rute Marques
References:
- Ângelo, D. F. (2020). A letter to the editor on “Root of helix inter tragus notch incision (RHITNI) for temporomandibular open surgery.” In International Journal of Surgery (Vol. 83, pp. 233–234). Elsevier Ltd. https://doi.org/10.1016/j.ijsu.2020.09.051
- Chakraborty, C. S. K. (2007). Eminectomy for the management of closed lock of temporomandibular joint. Medical Journal Armed Forces India, 63(4), 384–385. https://doi.org/10.1016/S0377-1237(07)80031-1
- Isler, S. C., Cakarer, S., Yalcin, B. K., & Sitilci, T. (2018). Management of the bilateral chronic temporomandibular joint dislocation. Annals of Maxillofacial Surgery, 8(1), 154–157. https://doi.org/10.4103/ams.ams_142_17
- Liddell, A., & Perez, D. E. (2015). Temporomandibular Joint Dislocation. In Oral and Maxillofacial Surgery Clinics of North America (Vol. 27, Issue 1, pp. 125–136). W.B. Saunders. https://doi.org/10.1016/j.coms.2014.09.009
- Martins, W. D., de Oliveira Ribas, M., Bisinelli, J., França, B. H. S., & Martins, G. (2014). Recurrent dislocation of the temporomandibular joint: A literature review and two case reports treated with eminectomy. In Cranio: Journal of Craniomandibular & Sleep Practice (Vol. 32, Issue 2, pp. 110–117). Chroma, Inc. https://doi.org/10.1179/0886963413Z.00000000017
- Mayrink, G., Olate, S., Assis, A., Sverzut, A., & de Moraes, M. (2012). Recurrent mandibular dislocation treated by eminectomy. Journal of Craniofacial Surgery, 23(5). https://doi.org/10.1097/SCS.0b013e31825ab523
- Pereira, J. V. C., Campos, G. S., & Paula, D. M. de. (2021). Surgical approach in Temporomandibular Joint disorders (TMJ): a literature review. Research, Society and Development, 10(13), e568101321711. https://doi.org/10.33448/rsd-v10i13.21711
- Stassen, L. F., & O’Halloran, M. (2011). Functional surgery of the temporomandibular joint with conscious sedation for “closed lock” using eminectomy as a treatment: A case series. Journal of Oral and Maxillofacial Surgery, 69(6). https://doi.org/10.1016/j.joms.2010.11.034
- Tocaciu, S., McCullough, M. J., & Dimitroulis, G. (2019). Surgical management of recurrent TMJ dislocation—a systematic review. Oral and Maxillofacial Surgery, 23(1), 35–45. https://doi.org/10.1007/s10006-019-00746-5
- Undt, G. (2011). Temporomandibular Joint Eminectomy for Recurrent Dislocation. In Atlas of the Oral and Maxillofacial Surgery Clinics of North America (Vol. 19, Issue 2, pp. 189–206). https://doi.org/10.1016/j.cxom.2011.05.005
- Vyloppilli, S., Joseph, B., Manojkumar, K. P., Sayd, S., & Krishnakumar, K. S. (2017). Surgical Correction of TMJ Bilateral Dislocation with Eminectomy and Capsulorrhaphy as an Adjuvant: Case Reports. Journal of Maxillofacial and Oral Surgery, 17(3), 345–349. https://doi.org/10.1007/s12663-017-1030-y
