Teething diseases
Машинный перевод
Оригинальная статья написана на языке RU (ссылка для ознакомления).
In the daily practice of an oral and maxillofacial surgeon, patients with dental anomalies are encountered.
These include:
Dystopia is a dental anomaly, which is characterized by the incorrect position of an erupted tooth.
Semi-retention is the incomplete eruption of a tooth.
Retention is a delay in the eruption of a formed tooth.
Read more about the classification of the position of third molars in the webinar Extraction of atypically positioned teeth: a piezosurgical approach.
Pericoronitis
Pericoronitis most often occurs when the lower wisdom tooth has difficulty erupting, but can also occur in the area of the upper wisdom tooth, premolars, and canines on both jaws. The eruption of the lower third molars occurs no earlier than 18–26 years, rarely occurs earlier than this period, more often later. Features of the anatomical structure of wisdom teeth are varied. They usually have fused or curved roots and well-defined rounded crowns.
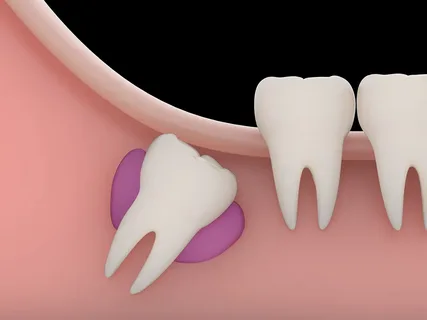
Rice. 1. Retention of the lower third molar.
Etiology
There is no temporary tooth in the area of eruption, therefore, the cortical plate here will be as dense as possible.
The thick mucous membrane covering the alveolar part includes fibers of the buccal muscle, which makes eruption very difficult.
Lack of space in the body of the lower jaw.
Pathogenesis
When the crown of the lower third molar erupts and the medial cusps are exposed, the unerupted cusps remain covered with mucous membrane, the so-called hood. According to studies, the contamination of mucous pathogenic microflora in the area of the hood of the wisdom tooth and the retromolar fossa is significantly higher than in other areas. The situation is aggravated by injury to the swollen and inflamed mucous membrane of the hood by antagonist teeth.
The purulent infection spreads in accordance with the anatomical features of the structure of the distal part of the lower jaw. So the retromolar region is rich in loose fiber, there is also a lot of it between the mucosa and the fibers of the buccal muscle, along the superior constrictor of the pharynx, at the posterior edge of the mylohyoid muscle.
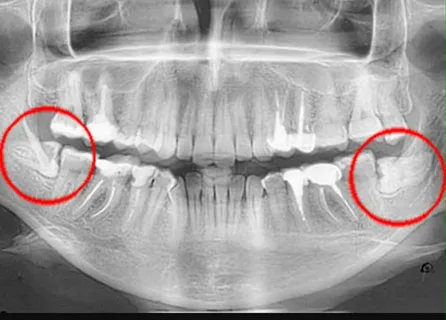
Rice. 2. Dystopia of the lower wisdom teeth on an x-ray.
Hence the most common complications:
acute purulent retromolar periostitis,
perimaxillary phlegmon and abscesses.
Classification
Forms of difficult eruption of the lower wisdom tooth:
acute pericoronitis, can occur in catarrhal or purulent form;
chronic pericoronitis;
retromolar periostitis.
Acute pericoronitis
Acute pericoronitis is a pathological process accompanied by inflammation of the gums and marginal periodontium around the wisdom tooth with difficulty in its eruption.
Etiology
Activation of the natural microflora of the mouth, where facultative anaerobes and anaerobes predominate.
Pathogenesis
In the area of the medial tuberosities, the mucous membrane is lysed.
The remaining part of the crown is covered with a mucous hood.
Under the hood and in the periodontal space, favorable conditions are created for the proliferation of microorganisms.
Injury to the mucous membrane of the hood during chewing causes erosion and weakening of local immunity.
The inflammatory process starts.
Clinical picture
Acute catarrhal pericoronitis . Opening the mouth is difficult, chewing is painful, the temperature is not elevated, and the general condition does not suffer. Lymph nodes may be enlarged and painful on palpation. Opening the mouth is moderately difficult. Locally, the tooth is located under a swollen, hyperemic mucous hood, the palpation of which is painless and there is no discharge. The prognosis is favorable, the process can be easily stopped with timely treatment.
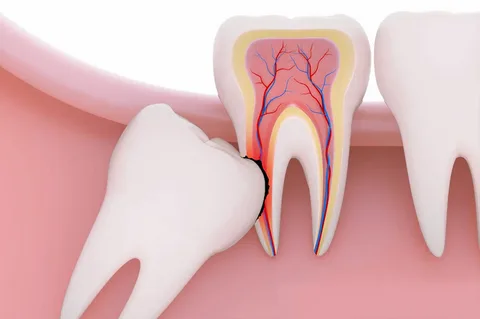
Rice. 3. Dystopia and impaction of the lower third molar.
Acute purulent pericoronitis . Occurs against the background of a deterioration in the general condition of the body, an increase in body temperature. It is characterized by severe pain in the distal part of the lower jaw, which is constant, intensifies when eating, and radiates to the temporal region and ear. Severe pain significantly limits mouth opening. Lymph nodes are painful and enlarged. The mucous hood is externally swollen and hyperemic. On palpation, a painful compacted infiltrate is revealed; if you press on it, a purulent discharge appears.
Chronic pericoronitis
The development of chronic pericoronitis occurs as a result of constant injury to the mucous hood by food or an antagonist tooth, due to frequent exacerbations of the inflammatory process. The accumulation of purulent discharge and the formation of granulations in the hood area causes local resorption of bone tissue.
Clinical picture
Chronic pericoronitis is characterized by variability in clinical manifestations.
Irradiation of pain to the ear and temporal region.
Unpleasant taste and odor from the mouth.
Enlarged and painful palpation of the lymph nodes.
Swelling and local hyperemia of the mucous hood.
Serous, and eventually purulent discharge from under the hood when pressed.
Painful palpation of the distal alveolar process of the mandible.
Frequent exacerbations of the process.
Treatment of pericoronitis
Therapy is aimed at stopping the acute process of inflammation.
Rinsing the sub-hood space with antiseptic solutions.
Dissection of the mucous hood along, exposing the crown, which avoids further accumulation of pus.
Antibiotic therapy.
After stopping the acute process, it is necessary to make a decision about the fate of the tooth itself.

Rice. 4. Indications for wisdom tooth removal.
If the wisdom tooth has the correct position in the bone and there is enough space for further eruption, in this case the doctor will completely excise the hood, freeing the entire crown.
If the tooth is in an incorrect position (dystopic) or there is not enough space in the bone for its eruption, its removal is indicated.
It is worth remembering that removing wisdom teeth during periods of exacerbation of inflammatory processes is not recommended.
Retromolar periostitis
This inflammatory process is the result of a violation of the outflow of pus during pericoronitis; the infection from under the hood spreads under the periosteum of the retromolar fossa and the tissue of the retromolar space, which leads to the formation of an abscess.
The clinical picture of the disease is similar to the manifestations of purulent pericoronitis, only all the symptoms are more pronounced.
Severe pain when opening the mouth and swallowing saliva.
The general condition suffers, weakness, fatigue, fever.
Swelling of the distal mandible.
Lymph nodes are enlarged and painful on palpation.
Mouth opening may be completely limited.
A painful inflammatory infiltrate from the retromolar region spreads to the outer, sometimes inner surface of the alveolar process of the jaw.
Principles of treatment
Treatment in a clinic setting.
Indications for wisdom tooth removal depend on its position in the bone and the availability of space for it, but removal is performed only after the acute process has subsided.
The incision is made from the pterygomandibular fold, its base, downwards, towards the arch of the vestibule of the mouth. In case of diffuse inflammation, the incision may end at the level of the molars.
Drainage is left in the wound, and daily dressings are prescribed.
Antibiotic therapy.
Eruption cysts
According to the results of ongoing studies, eruption cysts are observed in 30% of cases of difficult eruption of lower third molars. It is believed that the cause of the formation of the cyst is chronic pericoronitis; as a result of constant local inflammation, the mucous membrane peels off from the tooth.
Some authors believe that the formation of an eruption cyst is a consequence of the preservation of the embryonic epithelium, and the cyst is follicular (contains a tooth).
The clinical manifestations of a follicular cyst in the acute stage are similar to those of acute or exacerbation of chronic pericoronitis. The disease can be distinguished by an x-ray of the jaw branch taken in a lateral projection.
If the cyst is small, it is removed along with the wisdom tooth. If its boundaries extend to the ramus and body of the jaw, approaching the canal of the lower jaw, removal of the cyst and tooth is indicated in a hospital setting.
Technique for removing dystopic, impacted teeth
Local conduction anesthesia is performed.
The surgical approach is planned so as to minimize trauma to the bone and surrounding anatomical structures.
The vestibular approach is most often used, less often the palatal approach.
The mucosal incision must be sufficient to skeletonize the tissue in the area where the tooth is located.
The shape of the cut can be angular, linear or trapezoidal.
The mucoperiosteal flap is peeled off, the bone tissue over the tooth is removed with a drill.
Using an elevator, the tooth is dislocated and removed with forceps.
If possible, the wound is sutured.
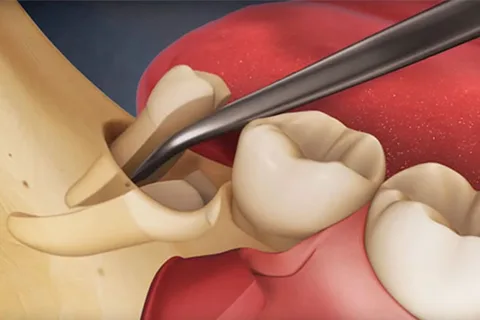
Rice. 5. Removal of the lower wisdom tooth.
If you liked this article, pay attention to the webinar Dental impaction: causes of development, anatomical prerequisites, instruments and surgical techniques .
